By Anna Nelson (@Anna_Nelson95) & Elizabeth Chloe Romanis (@ECRomanis)
In the previous post in this series we provided an overview of the problem of unconsented vaginal examinations during labour and reflected briefly on some of the key discussions and themes which emerged during our workshop. In this blog, we explore each of the three key themes in more depth. Our hope is that this reflection sparks further consideration and conversation about this issue and what can be done to tackle it.
- Listening to birthing people’s experiences is vital
Listening is clearly a means to prevent harm occurring in the first place. Where time and space are made for discussions of the purpose of vaginal examinations during labour before they are undertaken, birthing people are able to be genuinely empowered to discuss concerns or to meaningfully withdraw consent where they no longer find the procedure acceptable. There are, unfortunately, numerous examples of situations in which people had consented to examination initially but wished to either withdraw that consent, or to withhold consent to certain further procedures. For example, one participant shared the story of a woman who had initially consented to a vaginal examination but had then had her waters broken on the basis that the midwife ‘may as well while she was up there’. Had time and space been made for the woman to express how she was experiencing the situation; it is clear that she would have refused to consent to this.

Furthermore, listening is important because being silenced only compounds the harm that is done to people suffering the lasting harm of unconsented vaginal examination. Failing to listen also acts as a barrier to victims seeking whatever redress they desire – or even to realising that they may be entitled to seek redress. Finally, for the system to improve it is imperative that those who are performing vaginal examinations, and educating others about these (be that in healthcare schools or on birthing wards) do so from a place of understanding not only the medical utility of vaginal examinations, but also how these are experienced by the people upon whom they are performed – and the consequences of not adequately gaining consent or respecting refusal thereof.
- The importance of recognising harm
Though this bears similarities to the former theme; it is its own distinct issue. There are two central dimensions to the importance of affording due recognition to the harm experienced by a person who is the victim of an unconsented vaginal examination – the internal and the external. The internal element pertains to the anecdotal evidence that many people do not come to realise that harm has been imposed upon them until afterwards when they hear the stories / reflections of others. This links to the cultural expectation and the gendered normalisation of the ‘responsible pregnant person’[1] or ‘good mother’ submitting to whatever is presented as necessary by healthcare professionals to ensure that a ‘healthy baby’ is born, regardless of their feelings or preferences during the process of pregnancy and/or birth.

The external aspect of harm recognition encompasses the need for the birthing system to recognise that although vaginal examinations can be a valid procedure where fully free and informed consent is obtained, they can be extremely harmful where this is absent. There needs to be a far greater emphasis on quality consent to vaginal examinations. Even where consent is sought this does not mean that a person has been given sufficient information (explaining why the procedure is thought necessary as a matter of routine monitoring) nor has it been made clear that they can refuse permission. Further, the external aspect of harm recognition encompasses legal recognition of this harm and access (or lack thereof) to legal redress where desired. Law is a blunt tool, but it is often an important one for victims to know that the harm they have experienced is not ignored. Questions remain here though –vaginal examinations performed without consent are a criminal battery, but does using broad law constructed around general trespasses to the person do enough to recognise the harm that is actually incurred? It does not seem to adequately address some of the often gender-based elements to this crime, and the fact that an unconsented vaginal examination could be experienced as manifestation of abuse of power.
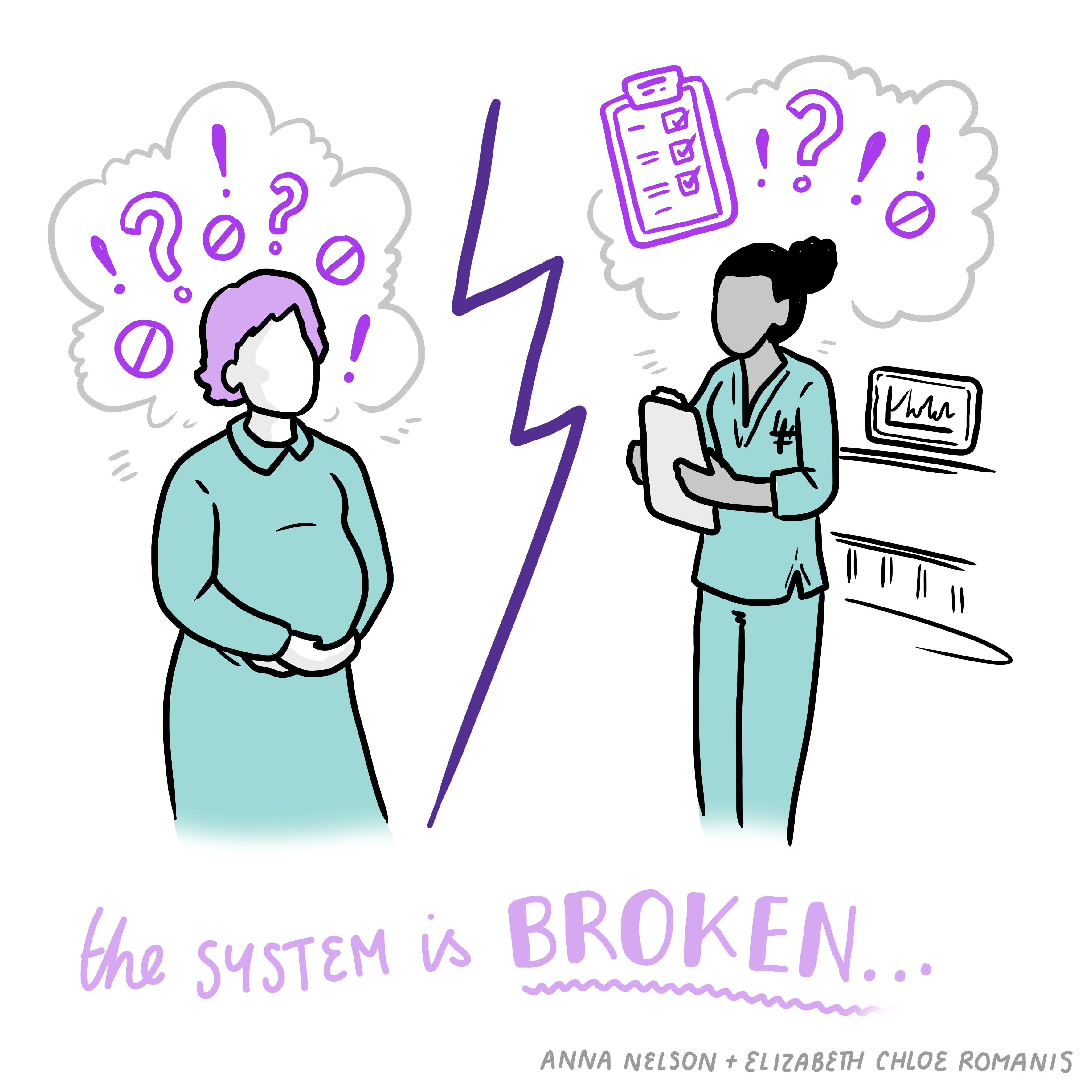
- The system is broken
The system under which healthcare professionals in pregnancy and birthing services work has a huge impact on the way they operate. Birthing services are underfunded, and (consequently) understaffed, and this impacts the quality of care they are able to offer. Time and staffing constraints, lead to an overemphasis being placed on the outcome of a healthy baby which fail to centre the birthing person and their needs and experiences. One participant reflected that the overemphasis was underpinned by lack of continuity of care. Where staff have time to get to know their patient they are far less likely to view them in the abstract, and are reminded and enabled to offer person-centred care based on discussions with, and the decisions of, the birthing person. Where continuity is interrupted as a result of broken systems and limited time, the person-centred approach is instead replaced with a ‘conveyer belt’ approach reiterating the notion that the priorities are healthy babies and efficiency. One participant midwife talked about how the system “took away the autonomy” of the midwife.
Systemic problems are also self-perpetuating. Problematic practices which develop under the pressures of the broken system become the norm – and these learned practices are passed down to those who are training to become healthcare professionals. One midwife reflected upon the fact that many universities do offer high quality training on the importance of obtaining meaningful consent for vaginal examinations, but that this gets overridden once students spend time on the wards and pick up learned habits from those around them.
However, while systematic problems do prevent good practice in many instances, we need to be careful that we do not allow the recognition of institutional problems to absolve individuals of responsibility where they are complicit in perpetuating a harm such as the performance of VEs without consent. Just addressing the problems of resources and funding will not – alone – automatically solve the problems of the normalisation of performing examinations on pregnant people without obtaining adequate consent. This has been normalised as a matter of healthcare practice and we need to work to ensure that this is changed from within.
[1] Deborah Lupton, ‘Precious cargo’: foetal subjects, risk and reproductive citizenship’ (2012) 22 Critical Public Health 329

Leave A Comment